Hemorrhoid Treatment
- Procedures
- Hemorrhoid Treatment
What Are Hemorrhoids?
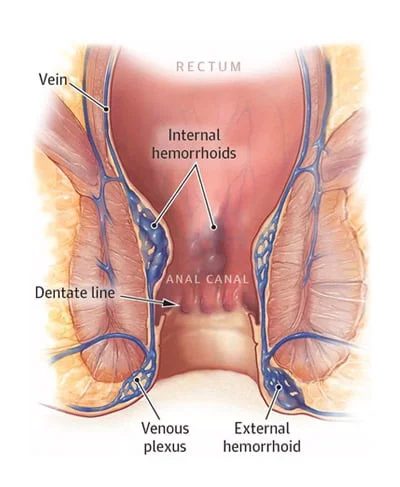
Hemorrhoids are swollen and inflamed veins that can cause discomfort and bleeding in the rectum and anus. If you suspect hemorrhoidal disease, you should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis, treatment plan and to exclude a serious illness or condition such as colon or anal cancer. Hemorrhoidal disease is just one of the many causes of rectal bleeding and lesions around the anus that need evaluation. Rectal bleeding can be a symptom of any type of colorectal or anal cancer, which can be cured if detected early.
Approximately half of the population develops symptoms of this health condition by age 50. Internal hemorrhoids form inside your anal canal, whereas external hemorrhoids form under the skin around your anus. If blood pools in an external hemorrhoid, it may form a clot called a thrombus. This condition can result in severe pain and inflammation.
What Are the Treatments We Offer at Midtown Endoscopy & Surgical Center?
Our Midtown Endoscopy & Surgical Center doctors are not only top-rated NYC gastroenterologists, but they’re also top-of-the-line hemorrhoid specialists. They offer a variety of hemorrhoidal disease treatments, including minimally invasive laser hemorrhoid treatments and other practical options.
In mild cases, topical medications and conservative treatment such as sitz baths and laxatives can help to alleviate symptoms. In other cases, we can perform IRC (Infrared Coagulation), hemorrhoid banding, or rarely surgery to remove the piles. A complete evaluation and diagnosis by your hemorrhoid doctor are very important for an accurate diagnosis and treatment plan.
When Should I See My Hemorrhoid Doctor?
If you observe blood when wiping or have discomfort and pain in your rectum, especially when you sit, you should see a hemorrhoid specialist. If your hemorrhoids start bleeding, your symptoms worsen, or they start interfering with your daily activities, visit a doctor right away. If you have a large amount of rectal bleeding (including painless bleeding) and dizziness, get emergency medical care immediately.
Whether dealing with internal or external hemorrhoids, choose a team of board-certified gastroenterologists specializing in diagnosing and managing the most common anorectal diseases, ranging from topical and medical therapies to outpatient treatments and surgical interventions.
What Are the Symptoms of Hemorrhoids?
Hemorrhoids have different symptoms and signs depending on the type, but the most common symptom is rectal bleeding when passing stools. Blood does not usually mix with the stool but coats the outer surface or is visible on toilet paper. The blood is usually a bright red and may be visible in the toilet.
Rectal bleeding, however, should always be evaluated by a physician or your local hemorrhoid treatment doctor, as it can be a symptom of a severe underlying condition, such as cancer.
Hemorrhoids can form inside your anal canal (internal hemorrhoids) or under the skin around your anus (external hemorrhoids).
How To Classify and Diagnose Hemorrhoids?
As part of your evaluation, our gastroenterologists will perform a thorough physical examination in our state-of-the-art facility, including a rectal exam and anoscopy. An anoscopy is a procedure in which a light-emitting device called an anoscope is gently inserted into the anus, allowing your physician to visualize the tissues in your anorectal area better.
Our GI doctors may also suggest a colonoscopy to see your colon in detail and to rule out other, more serious causes of your symptoms. A colonoscopy is the gold standard for visualizing the whole colon to make an accurate diagnosis.
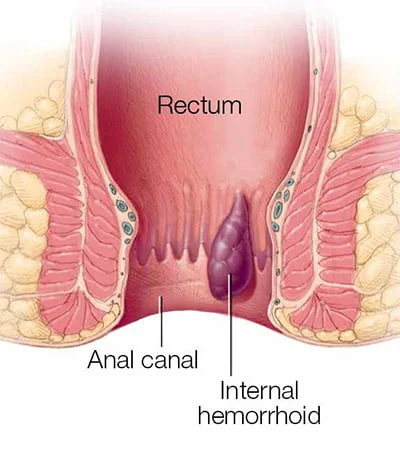
Internal Hemorrhoids
Internal hemorrhoids are located within the rectum and are not frequently felt or visible. You may bleed when passing a stool if you have internal hemorrhoidal disease. Hemorrhoids can push through the anal opening as a result of straining, causing irritation and pain when they prolapse or protrude. When the veins in your lower rectum or anus swell and bulge outward, you get a prolapsed hemorrhoid.
However, if internal hemorrhoid bleeding is causing you pain and discomfort, you should get medical assistance. A physician should evaluate your symptoms to ensure an accurate diagnosis and treatment plan and rule out serious illnesses or conditions such as colon or anal cancer.
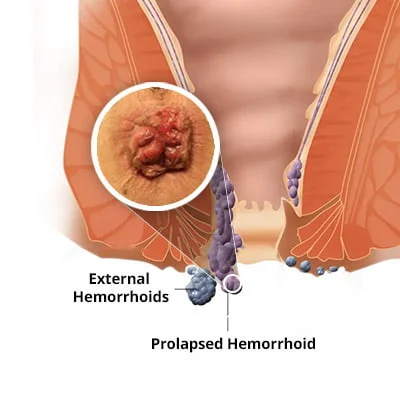
External Hemorrhoids
These are piles that develop beneath the skin surrounding the anus and can become thrombosed. You may notice signs and symptoms such as pain and bleeding. The area around your anus may be swollen. You may also have irritation or itching in the anal region. We recommend conservative therapies if external hemorrhoids become acutely thrombosed. A colorectal surgeon may refer you for excision in some instances.
Prolapsed Hemorrhoids
A prolapsed hemorrhoid occurs when a vein in your lower rectum or anus swells and creates hemorrhoids, resulting in an outward bulge. A prolapsed hemorrhoid can be very painful. The main symptom of a prolapsed hemorrhoid is the sensation of one or more lumps around the anus. However, this usually happens only if there is a significant prolapse.
It may be possible to push the lump back into the anus gently, but this merely changes the piles’ location and will not fix the problem. Prolapsed hemorrhoids tend to be quite painful when sitting and can hurt during bowel movements.
Protrusive hemorrhoids can collect small amounts of tiny stool particles and mucus, potentially causing pruritus and irritation. Unfortunately, continually wiping the area to relieve the itching can worsen the irritation.
What Causes a Prolapsed Hemorrhoid?
Hemorrhoids can prolapse when the connective tissues that hold them in place weaken. One possible reason is straining during bowel movements, which is especially likely if you have diarrhea or constipation.
Pregnancy also raises the risk, with up to 40% of pregnant women having hemorrhoids that can prolapse if left untreated. Another risk factor is obesity, which puts extra strain on the rectal veins, increasing the likelihood of piles and prolapsed internal and external hemorrhoids. Cigarette smoking can damage your blood vessels, including those in your anus and rectum, increasing your risk of hemorrhoidal disease and prolapsed hemorrhoids.
Thrombosed Hemorrhoids
If a blood clot or thrombus has formed within the prolapsed hemorrhoid, it can be excruciating. This is referred to as a thrombosed hemorrhoid. A thrombosed hemorrhoid can become acute and is more common in those who have severe constipation or a history of straining for long periods.
The pain is usually the worst within the first 24 to 48 hours. After this period, the thrombus is gradually absorbed, reducing pain. A thrombosed hemorrhoid can look like a blue-colored lump.
Although a thrombosed hemorrhoid isn’t as dangerous as developing blood clots in other areas of the body, you may require professional help to drain it and relieve severe pain. Prolapsed hemorrhoids can also be painful if they become strangulated, which occurs when the blood supply to the hemorrhoid is cut off.
Excisional haemorrhoidectomy is a surgical technique used to remove the excess tissue that is causing the bleeding. The surgery can be carried out under general anesthesia, spinal anesthesia, or sedation. It is a highly effective treatment for severe and recurring hemorrhoids, and it cures 95% of cases. The risk of complications is low. During surgery, one or more incisions are made near the hemorrhoid to remove it.
Hemorrhoid Treatment Options
Our doctors at Midtown Endoscopy & Surgical Center are top-rated New York City gastroenterologists and hemorrhoid specialists who offer varied hemorrhoidal disease treatments based on severity. In mild cases, conservative therapy may include sitz baths, laxatives, over-the-counter (OTC) or prescription medications. In other cases, we can remove the piles via IRC (Infrared Coagulation), hemorrhoid banding, or, in rare cases, surgery. A thorough evaluation and early diagnosis by your top hemorrhoid doctor specialist are necessary for an accurate diagnosis and treatment plan.
Our renowned gastroenterologists are among the best in the field, specializing in treating and preventing conditions related to swollen and inflamed veins in the rectum, referred to as hemorrhoids.
Please contact our office for more information about the best bleeding hemorrhoid treatment or to schedule a consultation with one of our hemorrhoid specialist GI doctors.
Laser Treatment for Hemorrhoids
While there are other methods for treating hemorrhoids, laser hemorrhoid removal is the most effective, fast-acting hemorrhoid treatment option. Our doctors have undergone special training in using IRC and have successfully treated many patients.
Laser hemorrhoid treatment uses infrared light, a laser, or an electrical current with the same efficiency. We conduct infrared coagulation on an outpatient basis in the center. We may administer mild sedation as necessary for the hemorrhoid laser surgery procedure, which usually only takes a few minutes.
The use of a laser for hemorrhoids has been shown to improve bleeding and pain in patients with internal and external hemorrhoids.
The laser hemorrhoid treatment procedure is more effective than rubber band ligation in reducing postoperative pain, resolving symptoms, and improving quality of life in patients with grade II or III hemorrhoids with incomplete mucosal prolapse.
What Is Infrared Coagulation?
The IRC, or infrared coagulator, contains a light source at its tip that applies heat to the hemorrhoid column’s base. This procedure causes scar tissue to form at the site, which can result in the hemorrhoid column diminishing or disappearing. This procedure is usually well tolerated with minimal side effects. Each treatment will only take a few minutes, and you may need several treatments to cover all areas. Patients can often return to work and other regular activities shortly after the treatment.
Why You May Need Infrared Coagulation?
Infrared coagulation is effective in treating both small and medium-sized hemorrhoids. If you have irritating internal hemorrhoids that continue to cause pain, bleeding, and other symptoms despite conservative treatment, IRC treatment for hemorrhoids may be the answer.
What Happens During the IRC Procedure?
During the infrared coagulation procedure, our hemorrhoid doctors use a handheld device that generates an intense beam of infrared light. A small probe is applied against the skin above the hemorrhoid, exposing the tissue to a quick pulse of infrared light. The infrared light’s heat burns the tightly targeted area, coagulating the vein above the hemorrhoid.
The resulting scar tissue cuts off the blood supply to the hemorrhoid, causing it to shrink and die—a scar forms on the wall of your anal canal where a hemorrhoid has formed. As an added benefit, the scar tissue holds nearby veins in place so they don’t bulge into the anal canal and become hemorrhoids.
Does Insurance cover IRC Hemorrhoid Treatment? Is It Painful?
Most insurances usually cover infrared coagulation treatment, and you won’t need an overnight stay in a hospital. IRC is more effective than sclerotherapy, and you may sometimes tolerate it better than rubber band ligation.
What Does Infrared Coagulation Preparation Involve?
In most cases, no preparation is required. Our hemorrhoid doctors will need to examine you to determine the best hemorrhoid treatment plan for your specific case.
What is Recovery like after IRC (infrared coagulation)?
It is expected to feel the need to urinate and experience minor rectal bleeding after each treatment. It is usually well-tolerated, but using a stool softener to help with bowel movements during healing can be helpful. Warm shallow baths, such as sitz baths, can also help in the healing process. Any symptoms that are concerning after your surgery should be discussed with your proctologist in NYC.
Laser treatment of hemorrhoids with IRC (infrared coagulation) is usually very well tolerated with minimal side effects.
What Are the Complications of Infrared Coagulation?
Although infection or bleeding can occur, infrared coagulation usually has few side effects or complications. Even though it is a relatively new technique, doctors have successfully used it to treat hemorrhoids across the country.
Hemorrhoid Banding
Hemorrhoid banding, also known as rubber band ligation, is a procedure in which a specialist uses a specialized instrument called a syringe ligator to wrap one or two tiny rubber bands around the base of an internal hemorrhoid. For this procedure, we use a banding kit accessory on the tip of a standard colonoscope.
The rubber bands are wrapped around the hemorrhoidal column, reducing blood supply and causing piles to shrink. Treatment usually takes only a few minutes, but if you have multiple hemorrhoids, the procedure may take a little longer. Rubber band ligation is a common approach for removing medium-sized internal hemorrhoids.
What is the recovery after hemorrhoid banding?
Treatment can be uncomfortable and cause bleeding at times, but the side effects are usually minor. To help prevent constipation, your doctor may recommend taking laxatives or using a stool softener. The bands typically pass with bowel movements once the piles have dried and withered. You should consult your doctor if you experience any troubling symptoms following surgery.
Surgical Options for Hemorrhoid Treatment. Do I need Surgery?
Only a tiny percentage of people require hemorrhoid surgery, and we will almost always prescribe it after other, less invasive procedures have failed. Sometimes, we recommend patients to a colorectal surgeon with whom we work closely. We can discuss the case with the surgeon to establish an effective treatment plan for your situation. You should discuss questions regarding further surgical options and recovery with your surgeon directly. We usually recommend surgery after less invasive procedures have been unsuccessful or are unlikely to be successful.
What is Hemorrhoidectomy?
Hemorrhoidectomy is a type of surgery to remove internal or external hemorrhoids that are extensive or severe. Although it is associated with the most complications, surgical hemorrhoidectomy is the most effective treatment for hemorrhoidal disease. An excisional haemorrhoidectomy is a surgical technique to remove excess tissue that is causing the bleeding. The surgery can be performed under general anesthesia or using spinal anesthesia or sedation. It is a highly effective way to treat severe and recurring hemorrhoids, and the procedure cures 95% of cases. The risk of complications is low. During surgery, one or more incisions are made near the hemorrhoid to remove it. The incisions are then closed or may be left open.
What Is Recovery After Hemorrhoidectomy Surgery?
You may be able to go home the same day as the surgery, or you may need to stay in the hospital for one night or longer. The incision may cause pain and bleeding for the first few days, and you may experience bleeding with bowel movements for several weeks after. Typically, 7 to 10 days off work are required.
What Is Stapled Hemorrhoidopexy?
Stapling hemorrhoids stop blood flow to the haemorrhoidal tissue and are typically used for prolapsed hemorrhoids.
Your doctor will administer general anesthetic, local, or spinal anesthesia before the procedure. You may feel some pressure during surgery if you choose local or spinal anesthesia, but you should not experience any pain. During surgery, the specialist uses specialized circular titanium staples to staple the hemorrhoid’s base to the rectum wall. Fibrous tissue develops around the staples during healing, which helps to anchor hemorrhoids in place, restricting blood flow to them and decreasing swelling. Eventually, the staples pass out with bowel movements.
What is Recovery After a Stapled Hemorrhoidopexy?
After surgery, you may need to spend a night in the hospital, and you may feel a sensation of pressure in your rectum for the first one or two days. During the first few days, you may have a small amount of bleeding from your rectum. Bowel movements may cause some bleeding and discomfort for several weeks.
How Long Do Hemorrhoids Last?
It is impossible to give an exact time frame. Everything is dependent on how severe the problem is. If your hemorrhoids are small, your symptoms may disappear in a few days without treatment. Making minor changes to your diet and lifestyle may also be necessary. Prolapsed hemorrhoids that stick out of the anus might require treatment from a specialist and will take longer to heal.
Some women develop this condition during pregnancy because of the increased pressure in the abdomen. In this case, signs of this health condition must appear after giving birth. Your best bet is to contact a leading gastroenterologist for an accurate and effective treatment.
Is It an Anal Fissure or a Hemorrhoid?
An anal fissure differs from piles in that it is a minor tear or cut in the anus lining. These are often confused, but their treatment is different. Anal fissures can result from sitting or passing hard or large stools. The lesion can cause pain and bleeding during or after bowel movements. Hemorrhoids differ as they are not tears in the lining but are swollen or dilated rectum veins. A trained gastroenterologist, who will perform a complete evaluation for a proper diagnosis and treatment, should diagnose and treat these conditions.
How Can I Tell If It Is Hemorrhoids or Cancer?
Both rectal cancer and hemorrhoids cause bleeding and other similar symptoms. If you suspect hemorrhoidal disease, you should always be evaluated by a physician for an accurate diagnosis and treatment plan, as well as to rule out a serious illness or condition. Hemorrhoids are just one of many potential causes of rectal bleeding and lesions around the anus that should be evaluated. Rectal bleeding can be a symptom of any type of colorectal or anal cancer, which is curable if detected early. There is, however, no reason to believe that having piles will result in colon cancer. However, never try to self-diagnose. An accurate diagnosis needs to be made by your physician.
Are There Any Specific Diets or Alternative Therapies for Hemorrhoids?
The most common advice for hemorrhoidal disease is to eat more fiber and stay hydrated. However, putting this advice into practice can sometimes be complicated. Consider aiming for 25 to 30 g of fiber a day. This amount is more than twice what the average American consumes. You should drink six to eight glasses of water and other liquids daily, excluding diuretics such as alcohol and coffee. Lifestyle changes are used in many alternative hemorrhoid treatments. As best-in-class gastroenterologists, our hemorrhoid doctors provide highly personalized and comprehensive care. Their philosophies regarding your best next step are based on trust, and they have challenged and established some of the most respected reputations in New York.
For more information about hemorrhoid treatment options or to schedule a consultation with one of our specialists, please contact our NYC gastroenterology office.